The Ultimate Guide To Eating Gluten-Free
Gluten-free may seem like the fad diet du jour. According to Harvard Health Publishing, there may be some evidence for this. Approximately 20-30% of the population does or has adhered to a gluten-free diet for some time, even though only 1% of the population is estimated to have celiac disease. Why the discrepancy? There's a lot of conflicting information about what gluten is and how it may or may not affect the human body.
Many jump on the gluten-free bandwagon because they heard from a fitness influencer or celebrity that it helped them achieve a fitness goal. Others believe it will help them with inflammatory conditions. Still, others may be affected by gluten hypersensitivity, which is a condition that still requires more medical research to define and explain.
Ultimately all of this talk about gluten has done one good thing for those needing to be on a gluten-free diet — it has expanded the awareness about the need for and availability of gluten-free foods and labeling. The days when a doctor would diagnose a patient with celiac disease and leave them feeling hopeless with a lengthy list of foods they can never eat again are long gone. Those who legitimately must be gluten-free can now live fuller, healthier lives. That said, there are some crucial things to understand when eating gluten-free is concerned. We are here to dispel some myths and provide some guidelines for those needing a gluten-free lifestyle.
What is gluten?
At its most basic level, gluten is a protein found in various kinds of wheat, including wheatberries, durum, emmer, semolina, spelt, farina, farro, graham, Khorasan wheat, and einkorn, rye, barley, and triticale, a hybrid of wheat and rye. Though oats are often lumped together in lists of gluten-free grains to avoid, oats themselves do not contain gluten. They can get broken down on machinery used to process wheat, meaning they can become cross-contaminated. While gluten is common in food products, like bread, pasta, and cereals, it is a hidden ingredient in myriad processed foods, cosmetics, skincare products, supplements, pharmaceuticals, and more, which makes it a challenge to avoid.
According to John Hopkins Medicine, when wheat gets ingested, various digestive enzymes, including the enzyme protease, spring into action to process it. Even though protease can break down most proteins effectively, it cannot fully process wheat gluten. Any unprocessed gluten will move through the digestive tract into the small intestine, where most people can pass it along with other undigested waste products.
The problem is that a small percentage of the population cannot pass the gluten. In the guts of these individuals, this undigested gluten can cause inflammatory responses associated with an autoimmune reaction. In other words, the body will assume the gluten is a foreign entity that is there to attack, which signals the need for natural defense mechanisms to get triggered. In essence, the body begins to attack itself.
What is celiac disease?
Celiac disease, also known as coeliac disease, celiac sprue, non-tropical sprue, and gluten-sensitive enteropathy, is a genetically transmitted autoimmune disease. Per John Hopkins Medicine, it affects approximately 1 in 100 individuals globally, or about 1% of the population, though medical professionals believe it is underdiagnosed by 70%. When someone has celiac disease, the villi, little hair-like filaments located along the small intestine, become inflamed due to the body's natural immune response against undigested gluten. This inflammation results in the malabsorption of nutrients and can cause a host of comorbid illnesses and symptoms.
Though there are over 200 symptoms associated with celiac disease, common ones include gastrointestinal discomfort, skin conditions, anemia, neurological issues, unexplained weight loss, mental health disorders, and failure to thrive in children, according to the National Celiac Association. Long-term comorbidities may include coronary artery disease, bowel cancers, type 1 diabetes, multiple sclerosis, osteoporosis, unexplained infertility, migraines, and more.
Celiac disease can only be diagnosed with a celiac-specific blood panel which detects specific antibodies associated with the condition, and a subsequent endoscopy with biopsies of the small intestine and duodenum confirming the diagnosis. Those who suspect they may have celiac disease should not discontinue eating gluten before or during testing, or they may obtain a false negative test result. The only verified treatment for celiac disease is to maintain a gluten-free lifestyle. There is no known cure. That said, once a gluten-free lifestyle is adopted, most individuals with celiac disease can and do go on to live healthy and active lives.
Who should eat gluten-free?
Contrary to popular belief, eating gluten-free is not recommended or advised for everyone. John Hopkins Medicine identifies three groups of individuals for whom a gluten-free lifestyle is necessary. These include those with celiac disease, wheat allergies, or gluten sensitivity. Though gluten sensitivity has been a hotly debated topic, there are some for whom consuming gluten can cause a host of both gastrointestinal and non-gastrointestinal symptoms but who do not fit the criteria for a diagnosis of celiac disease, according to Healthline.
A fourth group is also identified as needing to consume strictly gluten-free foods, those with a condition known as gluten ataxia, as stated in Beyond Celiac. Gluten ataxia is a rare neurological condition that may or may not be associated with a diagnosis of celiac disease. Individuals with this condition may experience symptoms including lack of coordination, dizziness, balance issues, problems speaking, and permanent damage to the portion of the brain responsible for coordination, the cerebellum.
Anyone who does not fit these criteria should not eat a gluten-free diet. Doing so may result in nutritional imbalances related to a lack of consuming vital vitamins and minerals in wheat, including fiber, B vitamins, iron, and magnesium. Additionally, many gluten-free foods are higher in calories, fat, sugar, and sodium, which may result in other medical issues ranging from heart disease to diabetes. And finally, gluten-free foods tend to cost more than conventionally produced foods. If you are concerned with health and wellness, try eliminating processed foods from your diet first.
Why do more people seem to have gluten intolerance?
There is a perception that more people are being diagnosed with celiac disease, wheat allergies, or gluten sensitivities than ever before. You may not be wrong. But why? According to Livestrong, some of the issues may have to do with disruptions in the microbiome of our guts. Our stomachs contain good bacteria that are integral to proper digestion. Any imbalances in the presence of these good bacteria due to the overuse of antibiotics and elimination of microbes from our foods may have decreased our capacity to process gluten.
Beyond Celiac suggests that there aren't more people with Celiac disease or gluten sensitivities, but awareness of and the ability to diagnose individuals effectively and efficiently have improved. Before the 1990s, blood tests did not exist to diagnose celiac disease. There was also an epidemic of misdiagnosis, where doctors thought symptoms had to do with other illnesses, not celiac. And finally, there may be environmental factors contributing, including an increase in gluten consumption, particularly among infants.
Lastly, according to Health Digest, there is a discrepancy between wheat produced in the U.S. and that grown in Europe. About 60% of the crop grown in the U.S. is a high-protein hard red wheat, while most grown in Europe is a soft or low-protein variety. This higher gluten content may be a culprit, but some evidence suggests a link to the herbicide glyphosate in American wheat. The belief is that this herbicide may disrupt our gut microbiome. For this reason, Glyphosate has gotten banned in several European countries.
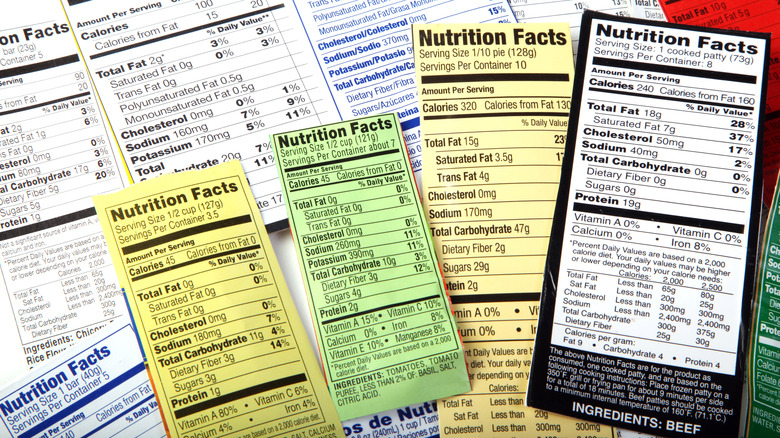
How to read labels if you are gluten-free
In 2004 the FDA passed the Food Allergen Labeling and Consumer Protection Act. This act requires all nine major food allergens to be labeled. These allergens are milk, eggs, fish, crustacean shellfish, tree nuts, peanuts, wheat, soybeans, and sesame. While this is a start, it does not guarantee something is gluten-free. First, it omits three important gluten culprits, rye, barley, and oats. It also does not cover foods regulated under the USDA, like produce, meat, poultry, egg products, and mixed products with more than 3% raw or 2% cooked meat. These are generally voluntarily labeled, but not always.
When reading labels, start with gluten-free, which indicates that a food item is likely safe for those with celiac disease. If there is no gluten-free statement, check the contains allergen statement for wheat. If wheat is not listed, you should still read the ingredient list to ensure no rye, barley, oats, brewers yeast, or malt extract are present. And then there are voluntary cross-contamination warning statements, such as may contain wheat or processed on equipment that handles wheat. Unfortunately, these are not regulated or required, but if you see one, the product is unsafe for those who must eat gluten-free.
If all else fails and you are unsure, look for products carrying a label indicating third-party certification, such as the Gluten-Free Certification Organization (GFCO) mark of distinction. These require products to undergo regular safety testing and verification that a product contains gluten levels of less than 10 ppm. The threshold for the FDA to label a food gluten-free is 20 ppm.
Sneaky ingredients that may have gluten in them
Reading nutrition and ingredient labels on food items is the first defense against accidentally ingesting gluten. That said, sometimes there are hidden culprits you may not know about. The Celiac Disease Foundation notes that if oats do not have a gluten-free label, avoid eating them. If gluten-free is not present on a packaged item, you should skip yeast extract, natural flavors, or rice syrup unless you can verify they are gluten-free with the food manufacturer. Foods that are regulated by the USDA, including produce, poultry, meat, egg products, and mixed products with more than 3% raw or 2% cooked meat that contain no allergen labeling, should be avoided if they have food starch, dextrin, spices, seasonings, or flavoring.
Some everyday food items that may contain gluten you should be particularly suspicious of are condiments, pre-made sauces, canned soups, salad dressings, seasoning blends, malt or distilled kinds of vinegar, flavored coffee or tea, licorice, cooking spray, and store-bought stocks or broths. Others include deli meats, imitation crab meat, sausages, vegan or vegetarian meat alternatives, jerky, and certain processed cheeses. If you aren't sure, it may be better to avoid a food item rather than take a risk and have a reaction, especially if you are highly sensitive.
Substitutes for flour in gluten-free recipes
When it comes to using flour in a recipe, the most common uses are as a thickener for a soup or sauce, as breading for chicken or fish, and as a binder for meatloaf or meatballs. Though you can find gluten-free substitutes that work one-to-one with regular flour, these often produce a less-than-pleasant mouthfeel in recipes. Some better alternatives exist depending upon the precise use.
When thickening sauces or soups, most recipes call for a roux or slurry prepared from flour to provide a smooth, luscious mouthfeel. To achieve similar results, consider puréeing some of the vegetables from your soup and adding them back into your soup, or add leftover mashed potatoes or yams. Another common thickener for sauces with a more neutral flavor is to combine cornstarch with stock or cold water and add it to your soup. A little goes a long way, and it will thicken as the soup simmers after adding it, so don't overdo it. And finally, you can try using various gums, like xanthan or guar, but be very judicious with these as they can quickly turn your soup into a coagulated mess.
For a substitute for breadcrumbs, either in breading meat or as a binder, you can use gluten-free breadcrumbs available at the market, but we prefer other gluten-free alternatives. Our favorite is ground nuts, which provide delicious flavor and a nice golden color when fried. Other preferred breadcrumb substitutes include pulverized gluten-free corn or rice cereal, potato chips, or toasted coconut flakes.
Tips for baking gluten-free
Though baking by weight is always a good idea, it is even more critical when measuring gluten-free flour, which can vary widely depending on brand and type. Baking is a science, and accuracy is crucial, particularly with gluten-free recipes. Get an affordable, reliable kitchen scale and use it.
Most gluten-free recipes require more moisture and fat to provide better texture, meaning baking times may vary wildly depending on your oven. Thus the amount of time a baked good has spent baking will be unreliable, as will your eyeballs. You will likely need to test the doneness of your muffin or cake with a skewer or a toothpick inserted into the center of the batter to ensure it is set. We also suggest adjusting oven temperatures by 20 degrees less, which will require longer baking times but will prevent your baked goods from burning on top before becoming thoroughly baked in the center.
Finally, gluten-free doughs and batters generally take more time and air to achieve maximum elasticity and the most tender texture. Unlike regular flour, which can be overworked, making it dense, gluten-free flour can handle rigorous and extensive mixing. Doing so will incorporate more air and encourage the ingredients to mingle. And before transferring your dough or batter to your baking pan or dish, let it take a sabbatical. Giving it 30 minutes to sit will allow the ingredients to homogenize, making your dough less gummy or toothsome.
Which gluten-free flours are best?
In the past, if you wanted to bake gluten-free, you had to create your blend out of six to eight different types of flours, gums, and starches that you would measure out carefully and have to spend hours stirring or shaking to mix thoroughly. Then you'd be left with bulky bags of partially used ingredients that would likely go rancid before you needed to make more flour.
Those days are gone. More options for gluten-free flours are available than ever, but not all of these are the same. We have found that while each states that it can be substituted one-for-one with regular flour, this isn't always the case. Some are better than others in terms of texture and taste. We have a few key criteria that are critical to consider.
First, we never use legume-based flour for baking. It tends to confer an unpleasant vegetable-forward flavor making the final product overly starchy. We also generally avoid gluten-free flour blends made of predominantly coconut flour or cassava flour, as these both tend to weigh down the final product. Finally, though some of the best quality gluten-free flour blends contain dairy powder, we usually skip these. Many who avoid gluten also cannot tolerate dairy.
Our favorite blends contain brown or white rice flour as a base, with sorghum flour, potato, tapioca starch, and a binder, such as xanthan or guar gum. For savory dishes, buckwheat flour or quinoa flour may be suitable, but these tend to be overly bitter in sweeter baked goods.
Can I drink alcohol if I'm gluten-free?
According to Beyond Celiac, distilled liquor is gluten-free, even if produced using wheat, rye, or barley. While this may sound counterintuitive, according to the Alcohol and Tobacco Tax and Trade Bureau (TTB), liquor that has undergone thorough distillation has all protein eliminated, including gluten. The absence of gluten is scientifically provable, and as long as the manufacturer can guarantee that there is zero chance of cross-contamination that may occur throughout the entire production process, the distilled liquor may be labeled gluten-free. Examples include bourbon, scotch, vodka, and whiskey, which may get produced from wheat. Though for those who remain concerned about trace amounts of gluten or cross-contamination, there are plenty of options, such as gluten-free vodka made from potatoes and whiskey made from corn.
Fermented alcoholic beverages undergo a different production method, which does not remove gluten. For this reason, fermented alcoholic beverages produced using wheat, rye, barley, or any other gluten-containing grain should be avoided. These include most beers, though myriad gluten-free beers and ciders are available. Wine and champagne are almost always considered gluten-free. As a general rule, we recommend avoiding cocktails made with various mixers, as many of these can have added gluten.
What about gluten-free pasta?
Pasta is one of the foods that are a luxury item for those needing to eat gluten-free. Though there are more gluten-free pasta options now than ever before, if we are being honest, most of them are very poor facsimiles for pasta that cost a lot and are inferior. Many gluten-free pasta brands are gummy, fall apart, and have bizarre flavor profiles that make them unpalatable. That said, we have found a few that were to our liking.
Generally, we prefer gluten-free pasta made with corn or a corn and rice hybrid. These tend to have the best texture and will hold their shape, particularly when topped with denser sauces or used in pasta salad. We almost always avoid legume flour or vegetable-based pasta as they frequently have a weird aftertaste that tastes like dirt and a very starchy mouthfeel that can be unpleasant. They also can cause gastrointestinal discomfort, which may completely negate the whole point of eating gluten-free in the first place.
When it comes to dry pasta, we almost always default to Barilla gluten-free pasta. It is consistent and has a flavor that is similar to regular pasta. A quality fresh gluten-free pasta that we were rather impressed with was the basic pasta shapes made by Taste Republic. Their fusilli, linguini, and fettuccine noodles had superior texture and flavor and held up beautifully to myriad sauces.
What about gluten-free bread?
Bread is a staple of many diets, so finding one you can incorporate into your daily life when you need to eat gluten-free is crucial. Several factors go into good quality gluten-free bread. Because gluten helps provide an elastic texture to regular bread, most gluten-free bread can be a disappointment compared with the real deal. They tend to be denser and lack the fluffiness we associate with plain white bread. For this reason, you should look for gluten-free bread that has a good combination of flours for flavor, along with various starches and gums for texture.
Gluten-free bread also tends to be paler than regular bread unless it has been encouraged to form a crust with an egg wash. For this reason, it lends itself to being toasted more than eating straight out of the bag. That said, we have found some that are serviceable for sandwiches. These usually contain some corn flour in them. We recommend avoiding legume flour-based bread as they have an aggressive vegetable-forward flavor that can overwhelm your palate, and some have a grainy texture.
And, finally, gluten-free bread doesn't have a long shelf-life. Nothing is more infuriating than spending a small fortune on a loaf of gluten-free bread that becomes moldy within a day or two. This is why so many gluten-free bread brands are sold frozen or in vacuum-sealed plastic containers. If you don't eat bread frequently, we suggest leaving the loaf frozen and removing a piece or two at a time as needed rather than thawing it all at once.
Tips for eating out if you are gluten-free
The process of eating out used to be almost impossible if you required a gluten-free menu. Most restaurants did not have the information, knowledge, or capacity to accommodate those with gluten allergies. Fortunately, times have changed, with myriad websites and apps having lists of restaurants that not only have gluten-free menus but have been tested for quality and safety by others needing to eat gluten-free. That said, there are still some precautions to take when dining out.
When you arrive at a restaurant, ask for a gluten-free menu or if gluten-free dishes are designated. Let your server know that you require a gluten-free meal so that they can flag your order for the kitchen staff. Doing so will usually trigger them to swap out utensils and cookware for fresh ones and to clean any surfaces properly to avoid cross-contamination. Speaking of cross-contamination, find out if there is a designated fryer for those needing gluten-free meals. Fryers are often the most overlooked and common culprits of cross-contamination.
And, finally, don't be afraid to ask questions. A server may not know all the answers to whether or not a particular sauce or soup has flour in it, but they can and should confer with the kitchen staff. In our experience, even items listed as flourless, like a cake, may have had flour added to them in the form of the pan in which they baked. It doesn't hurt to be overly cautious, and restaurants do not want to risk accidental glutening of a customer.
Entertaining gluten-free
One of the settings that can be the most frustrating and deflating for someone needing to eat gluten-free is social settings where there will be food. Having to navigate whether or not to eat before you attend, if you should bring a dish for yourself, whether you can trust those hosting to prepare your food safely, and how much time you want to spend discussing your condition are all factors. From the host's perspective, there are some basics you can do to take the stress out of the equation for yourself and for those in attendance who need to eat gluten-free.
Our first recommendation is to make everything on the menu gluten-free. There are plenty of foods that are naturally gluten-free without needing much by way of alteration. Providing everyone with the same menu alleviates additional stress or danger for all parties involved, and nobody will ever know the difference. If you plan to have gluten-free and non-gluten-free items, make sure these are clearly labeled for ease so that nobody gets accidentally glutened. And finally, make sure you take plenty of precautions in preparing the meal to avoid cross-contamination. These included cleaning thoroughly and not preparing gluten-full and gluten-free dishes simultaneously.
One final note to help facilitate gluten-free entertaining. Always cook from scratch, and stock your pantry with gluten-free ingredients. All condiments, spices, oils, vinegar, and more should be gluten-free. Doing so will eliminate the need for second-guessing yourself and make the cooking process far less complicated.